(I wrote this after being approached by Love What Matters after they saw one of Noah’s Batman pictures and wanted to publish his story.

July 26, 2018
As I find myself sliding down the wall to the ground, I think to myself, “I can’t believe my son is going to die on my birthday”, only it’s not just a thought as I realize that I moaned this out loud. . . and really, who thinks thoughts like that when their son is down the hall dying? I don’t think there is probably a right or wrong way to react in a moment like this, but I’m convinced that if there IS a wrong thing to think, this would be it.
Through a distant fog I hear my ex-husband, who is crying next to me, tell me to “STOP, it’s going to be ok!”, but as I wrap my arms around my head to try and block out the brutal unfairness going on around me, all I can see when I close my eyes is Noah’s eyes going blank and him slumping over as he starts seizing. . . . . and all I can hear, ringing over and over again in my ears is the monotone voice over the loudspeaker saying “Medical Alert. Code. Room 204 . . . Medical Alert. Code. Room 204.” This can’t be happening, again.
Even though my 12 year old son has lived with his heart condition his entire life, there is still nothing that prepares you for a moment like this.
November 27, 2005
We found out at our 20 week ultrasound that our baby boy was going to be born with a Congenital Heart Defect called Hypoplastic Left Heart Syndrome (HLHS). This is a heart defect in which the Left Ventricle doesn’t form in utero. This was devastating to me. What do you do with information like this? When they first told us, I didn’t know if my baby was going to live or die. Not knowing is the worst!
At the time we saw a multitude of specialists, cardiologists and surgeons and we were given three options. Heart Transplant, 3-stage open-heart surgeries, or “Comfort Care”, which means we keep our baby comfortable until he dies. I think we deliberated for about 2 seconds before we opted for the 3 stage surgeries. Both Noah’s dad and I felt that it was best to be pro-active rather than to wait for that terrifying unknown.
Noah sailed through his Norwood procedure when he was 5 days old, his bi-directional Glenn when he was 4 months old and his Fontan just before his 3rd birthday. The only complication he ever had was a nicked nerve which affected his vocal chords for a few months.

When I look back at that time, I honestly feel pretty nonchalant about it. We all just did what we had to do. There was never another option. There was never a pause. We just plowed through it, dealt with everything that was thrown at us and treated Noah like a normal kid, with some minor limitations. Other than our yearly cardiology visits and the occasional winter ER visit, Noah has been as healthy as one with half of a heart can expect to be. I mean, it’s not like I never thought about it. Noah has always had some limitations and considerations. He qualified for a Make-A-Wish to go to Legoland, California when he was 8. He attends a camp just for kids with heart defects, and he turned blue when cold. Other than that (and the 8” scar down his chest) you would never even know he was a “heart kid”. He’s just a normal kid who fights with his brothers, is obsessed with Legos and Star Wars and wants to be a zoologist when he grows up.
Which is why I am still feeling so much shock, and residual fear, over what happened. Almost a year later I still find myself having nightmares about all of the “what-ifs” that could have happened if Noah wasn’t in the exact place that he was at the time his heart decided to quit working properly.

July 21, 2018
My friend who is watching my kids while I’m shooting a wedding calls me. We joke around a lot, so I answer the phone, “Hey!! Everyone still alive?!” in a hardy-har sort of voice. My best friend (former pediatric nurse) quickly says “Yes, but actually Noah passed out up in the tree fort and he’s really lethargic and . . . .” and I can’t remember what else she says as my brain starts going into freak out, ‘oh shit, is this really happening?’ mode. Something happening to Noah has always been in the back of my mind as one of those worst fear type scenarios, but naively, I believed in my own heart that he would be “healthy” forever.
I quickly tell her to take him to the ER and she assures me they’re already heading out the door. I hang up the phone and I call my ex-husband and ask him to meet them at the ER.
At this point, not knowing how bad it is, I decide that I have to stay and do my job. I tell my Second Photographer what’s happening. I tell the wedding planner, so she knows why I am stepping out every 5 minutes to look at my phone.
I feel powerless.
I’m terrified, but I’m determined to get through the next hour, so I’m literally shooting with one hand and watching my phone for texts from my ex-husband in the other hand.
Then he texts me:
“ Blood and ekg. Maybe you should let them know you should leave. He is really cold and heart rate is fluctuating 40-30” I can only respond “Ok”. Then I get another text that just says, “.4 of atropene, Epi now.” At this moment, I know this is bad. I have to leave, now. My second photographer and another photographer friend who was officiating the wedding cover the last half hour for me, and I leave in my friend’s car.
I feel SO far away from my son right now. It’s an hour drive from Omaha to Lincoln and I don’t know how I’m going to get there with my heart racing and tears streaming down my face. I’m supposed to be with my son when he’s hurt. That is the job I signed up for when I birthed him and now I’m not there for him. Is he scared? Is he in pain? How can I protect him when I’m so far away? I’m almost out of town and my ex-husband calls and tells me to turn around and go to Omaha Children’s Hospital. They’re life-flighting Noah there.

I’m now in the PICU waiting room and I wait nearly an hour for the helicopter to get there. They finally come out and tell us that they have Noah and he is currently stable. They say they are going to take him down to do an emergency cath, but I can go back and see him before they go down. As we’re talking to the anesthesiologist about the procedure, the Cath doctor rushes out to the waiting room and says there is a change of plans, they need to go, NOW. The anesthesiologist and cath doctor rush away and my own heart drops for the umpteenth time that night. In less than a minute, we hear, for the first time, “Medical Alert. Code. Room 204 . . . Medical Alert. Code. Room 204.” my ex-husband and I grab each other and we sink to the floor together, sobbing. Again the powerlessness; that desperate feeling that I need to protect my son and I can’t. I wonder if I will see my son alive again. I mentally go through our morning interaction, and I wonder if that was the last hug I would ever give him.
After several hours, and probably too many cups of coffee later, they’re done with the emergency heart cath at about 4 am. They put in a temporary pacemaker and we finally get to go back and see Noah. He is sedated and paralyzed (to prevent any movement from displacing the cath in his groin) and he is on the ventilator. . . but he is alive and breathing, so I can breath again, too.

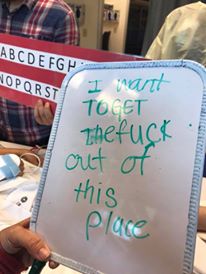
Over the next couple days, Noah is in the process of getting weaned off the ventilator. He is in and out of consciousness, and when he’s awake it’s hard for him to cope with the tube down his throat. He tries to communicate with us and he is clearly confused and trying to talk around the tube. I hold his hand and smooth his hair back. The speech therapists bring in a laminated sheet of letters for Noah to point at one by one to try and let us know what he needs. One by one he points and I write the letters down on a white board. At the point Noah points to an F and then a U, I start laughing because I already know where this is going and I can’t even be mad at him.
Painstakingly, Noah points to every single letter to spell, “I want to get the fuck out of this place.” At this point, the nurse who was working the first night Noah came in tells us how Noah was talking with everyone when his heart stopped. Dr. Sid, who had his hand on his chest and felt it stop, gave Noah a couple quick chest compressions, and Noah wakes up, shoves his hands away, and yells “STOP THAT!” In all of the fear and anxiety, these little stories and moments show me just how strong Noah is.
When Noah’s heart function did not fully return the next couple days, they decide to put in a permanent pacemaker. The surgery went great and all seemed well, until the cardiologist came in and told us to sit down. We all know that’s not a good sign, and I think, “NO! This isn’t fair!!” I wanted to stop him from telling me whatever he needed to tell me, but my heart is in my throat and I can’t speak.
He tells us Noah has a clot. They need to start Noah on heparin and TPA to try and dissolve the clot. They want to push the boundaries with this.
The risks?
Excessive bleeding. The clot dislodging and going to Noah’s brain. . . etc. etc. “Ok,” I think “This is where we are and this is what we need to do”. I try to stay calm and to be strong for Noah because I don’t want to scare him. He’s only 12, and I don’t do a great job of hiding my red rimmed, tearful eyes from him. He’s a smart kid, and I could tell that he knows it’s not great.
His dad brings in a “worry doll” that is supposed to eat your worries so you don’t have to keep the worry inside. I’m sitting beside Noah on the bed when he writes down his worry, and my heart lurches into my throat. I didn’t mean to look, but I see Noah write, “I don’t want to die” on a little piece of paper and put it into the worry doll’s mouth. I hold him and tell him that if he is scared about anything, including dying, he can talk to me or his dad about it. I silently plead, “Please don’t keep that fear inside of you, baby boy. You don’t have to deal with this yourself. “

Back to July 26, 2018
. . .Noah comes back from a CT. The nurses are talking by their computer and I go to get Noah a glass of water. As I turn around with his water I see Noah’s eyes go blank, I see him slump over and he starts seizing. . .
I’m now down the hall and as I’m sitting on the floor by my ex-husband, watching the doctors and nurses going in and out of the room, I feel totally numb. Another kid’s parents start down the hall and stop, looking at the commotion in front of them, clearly not knowing where to go. All they want to do is get to their own child, and there are too many people to get through. I watch them and feel a hysterical laugh work up into my throat. I want to tell them not to worry. It probably won’t happen to their kid. This kind of thing doesn’t REALLY happen to people.
. . . I read in the notes almost two weeks later that Dr. Kelly did about 5 minutes of CPR on Noah. He had a stroke and a heart attack and his heart tried to stop on him, but his doctors weren’t going to let him die. Noah clearly wasn’t about to give up, either.
After they revive Noah they start checking his neurological status because they’re worried that the clot that went to his brain may have caused significant brain damage. He is back on the vent with a large incision near his groin in the case they need to put him on life support and the neurologists are in the room, trying to see if there is any brain activity. I walk into the room and I grab Noah’s hand and start talking to him and his head turns toward me!!! Noah heard me and all of the doctors in the room cheer and tell me what a great sign this is!! When asked, Noah squeezes my hand and by the next day another CT shows the clot in his brain is resolved and gone! I feel that a miracle just happened and Noah is going to be ok!


Noah decided to get well about as fast as he got sick. Three weeks after Noah was admitted to the hospital they tell us to pack our bags, were going home! Noah went home with a pacemaker, several more meds and a Coumadin prescription that needs to be closely monitored, but Noah is the most amazing and strong human that I know and I’m positive he will continue being brave and strong and get through anything that comes at him.
This seems like an insane and weird revelation, but life seems so real to me now and Noah has reminded me that I don’t get to take even one second of it for granted. If my hero won’t let a little thing like two codes, a pacemaker surgery, a clot, a stroke and a heart attack keep him down, I do not get to complain about any number of the first world problems that I have. I get to live life with Noah as my guiding inspiration, and for that I’m grateful.







(Update: About 3 months after this event, the doctors decided to list Noah for a heart transplant. After only 5 days of being on the transplant list, Noah received his new heart, on November 11, 2018, just two weeks before he turned 13. He is currently doing AMAZING!)
Be the first to comment